Making Vitamin D Work Smarter, Safer, and in Context
We hear warnings about sunlight, but rarely about supplements. Vitamin D isn’t just a “nutrient pill” — it acts like a hormone that influences our immune system, blood pressure, and metabolism. Our skin has built-in safety brakes for making vitamin D from the sun, while supplements can bypass those brakes. That’s why conversations about vitamin D from sunlight vs supplements are so important. This guide explores how both play a role — and why balance is the key to making vitamin D work for us.
🔑 Key Takeaways
- Sunlight safety: Sun doesn’t cause vitamin D toxicity — your skin photodegrades excess vitamin D; supplements are where toxicity happens.
- Dose caution: High-dose D isn’t always helpful. Without the right foundation (magnesium, inflammation status, conversion balance), big doses can backfire.
- Hormonal role: Vitamin D is a hormonal signal. Once activated, it influences immunity, metabolism, and the renin–angiotensin system (blood pressure regulation). Supplementing without considering the bigger picture can disrupt feedback loops.
- Smarter testing: Don’t just check vitamin D storage (25(OH)D). Also consider the active hormone (1,25(OH)₂D). Think of it like your money: 25(OH)D is the savings account (what’s stored), and 1,25(OH)₂D is the checking account (what’s being spent). Looking at both — and their ratio — gives a truer picture.
- Magnesium matters: It’s a cofactor for vitamin D activation; low magnesium can make D supplementation feel worse.
- Light rhythm: Sunlight + circadian rhythm support vitamin D biology in ways a pill can’t replicate.
🍀 Why Low Vitamin D Needs Context
Vitamin D does far more than support bones. It strengthens the immune system, steadies hormones, and even influences mood and energy. It helps cells “talk” to each other, guides how calcium is used, and supports heart, muscle, and mitochondrial function. But as important as it is, more pills aren’t always the answer — the bigger picture matters. Recent studies show that vitamin D works across both the body’s first-line defenses (innate immunity) and its long-term memory (adaptive immunity). [8]
Here’s an example: some people with thyroid issues, inflammation, or energy stress show low 25(OH)D (low savings) but normal or high 1,25(OH)₂D (active spending). This doesn’t always mean true deficiency. Sometimes the body is shifting how it uses vitamin D as a short-term coping strategy. In those cases, adding more vitamin D can create extra strain rather than relief. [7]
That’s why before adjusting, it’s wise to pause and see the system as a whole. What looks like a “problem” on a lab result may actually be your body’s way of protecting itself for the moment.
🔔 Vitamin D as a Hormonal Signal
Once vitamin D is activated to 1,25(OH)₂D (the checking account form), it behaves more like a hormone than a simple nutrient. It helps fine-tune gene activity — turning some processes up, quieting others down — to guide immunity, metabolism, and the body’s balance of fluids and blood pressure.
One clear example is its role in the renin–angiotensin system (RAS) — the hormone network that helps regulate blood pressure and fluid balance. At the front of this system is renin, an enzyme from the kidneys that acts like a starter switch. It sets off a chain reaction that can narrow blood vessels and raise blood pressure. Vitamin D helps by easing this system when it’s running too high.
Why does this matter? Because an overactive RAS can drive chronic high blood pressure, strain the heart, increase kidney risk, and damage blood vessels over time. Vitamin D’s hormonal role can help steady the system — but too much supplementation can pull on this lever in unintended ways. [4,5]
- Cardiometabolic signal: Low vitamin D is linked with higher cardiovascular risk. While correlation isn’t the same as causation, part of this connection may come from how vitamin D interacts with the RAS and blood pressure regulation. It’s another reminder that vitamin D affects the whole body, not just the bones. [4,9]
- Mechanistic check: The active form 1,25(OH)₂D can dial down renin when it’s running high — helpful when the system is overactive, but over-supplementing can tip the balance too far and disrupt the body’s feedback loops. [5]
In short, vitamin D’s influence ripples through hormonal networks, showing why it acts more like a hormone than a simple nutrient. A 2025 review reinforced this, highlighting links between vitamin D status and cardiovascular outcomes, and underscoring how its effects extend well beyond bone health. [9]
🌱 Magnesium: The Essential Partner
Magnesium is the quiet partner that allows vitamin D to do its job. It helps the body activate vitamin D and also supports hundreds of other processes tied to energy, mood, muscles, and sleep. Without enough magnesium, vitamin D can feel more like a stressor than a helper.
Many of us run low on magnesium because of modern diets, depleted soils, and everyday stress. If you add vitamin D on top of low magnesium, you may notice fatigue, anxiety, cramps, or poor sleep — not because vitamin D is “bad,” but because the supporting partner is missing. [6]
Practical ways to support magnesium include eating more foods rich in it — such as pumpkin seeds, cacao, leafy greens, avocado, and almonds — and, if needed, discussing supplements like glycinate, malate, or threonate with your practitioner, especially if you’re also taking vitamin D. [6]
🧪 Testing: Reading the System, Not Just One Number
Before we dive into patterns, let’s unpack what these two markers actually mean.
🧮 Storage vs. Active Vitamin D
- 25(OH)D (calcidiol): This is your savings account. It’s the stored form, sitting in reserve. Doctors most often measure this one because it reflects overall availability. But just like money in savings, it doesn’t always show what’s being actively used.
- 1,25(OH)₂D (calcitriol): This is your checking account — the active, spendable form. It’s what your cells actually use to regulate calcium, support immune defense, and influence energy metabolism. Even when savings (25(OH)D) look low, checking (1,25(OH)₂D) can already be running high, especially in chronic inflammation or mitochondrial stress.
Measuring only 25(OH)D is like looking at your savings balance without ever checking your checking account. You might assume you’re broke when money is actively moving — or the reverse: plenty in savings, but very little in circulation.
🔄 Why the Ratio Matters
Most standard panels only measure 25(OH)D (savings). But in more complex cases — autoimmunity, persistent fatigue, or unusual symptom patterns — adding 1,25(OH)₂D gives important insight. Looking at the ratio between storage and active forms helps reveal how the body is regulating vitamin D.
- Low savings + High spending (Low 25(OH)D + High 1,25(OH)₂D): This pattern often shows up when the body is under stress — from ongoing inflammation, hidden infections, or energy struggles in the mitochondria. It’s like your checking account is working overtime even though savings are low. In this case, adding more vitamin D can sometimes add fuel to the fire instead of helping. [7]
- Low savings + Low spending (Low 25(OH)D + Normal/Low 1,25(OH)₂D): This pattern looks more like a true shortage — both savings and checking are running low. Here, carefully rebuilding vitamin D stores (with proper guidance) may give the body what it’s genuinely missing.
👉 Lab handling note: The active form of vitamin D (1,25(OH)₂D) is more delicate, so accuracy depends on how the sample is handled. That’s why it helps to use reputable labs with strong practices. As of the time of this writing, major labs such as Labcorp, Quest Diagnostics, and Mayo Clinic offer high-quality vitamin D testing. Each has LC-MS/MS assays available (the most precise, since they separate vitamin D₂ and D₃), though automated methods are also common. These labs typically refrigerate samples short-term and freeze them for longer transport — but since protocols can change, it’s always wise to confirm details with your lab so you know exactly how your sample will be processed.
💭 Good questions to ask:
How long is the sample stable during transport?
Do you freeze the sample if it can’t be tested right away?
Which method is used — LC-MS/MS or an automated test?
📊 Labs to Consider
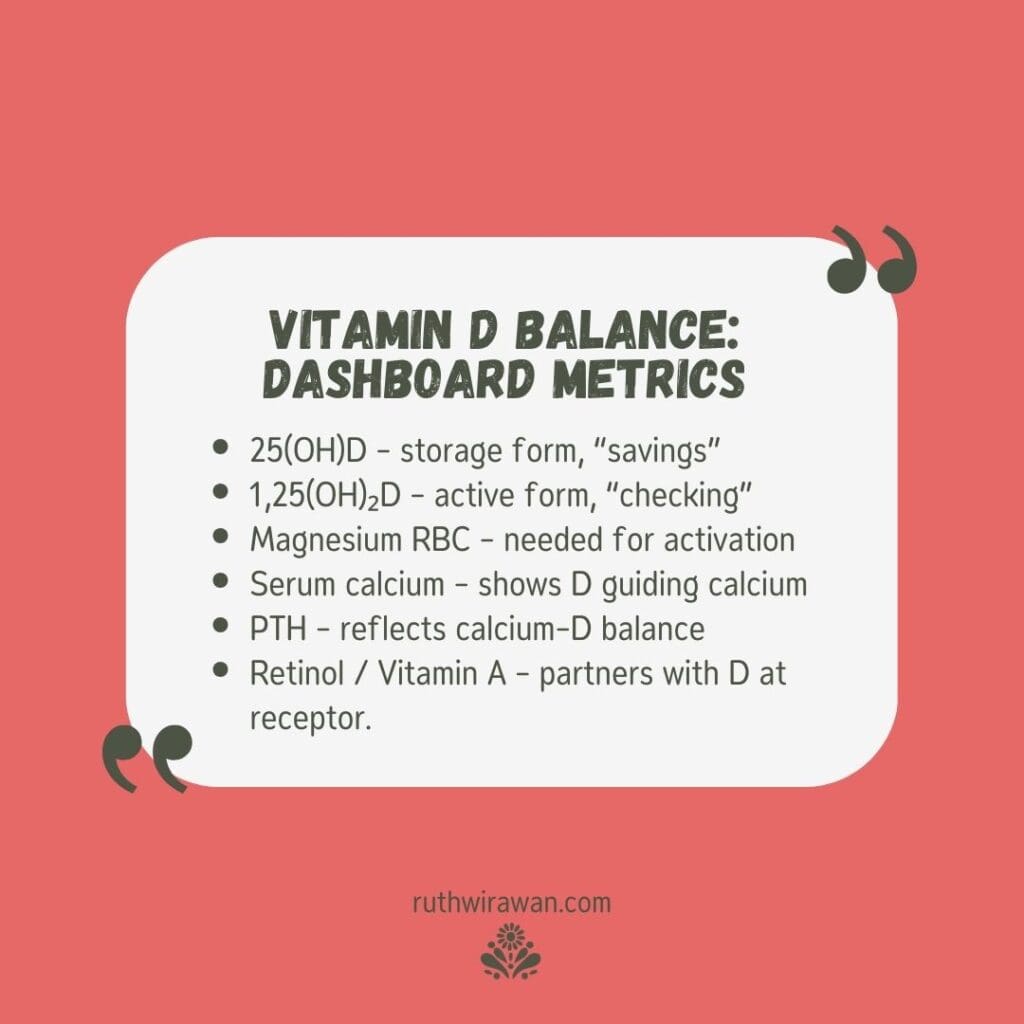
Measuring only 25(OH)D gives an incomplete picture of vitamin D status. Instead of stopping there, a more complete panel combines both storage and active vitamin D with vitamin A, magnesium RBC, serum calcium, and PTH. When viewed together, these labs reveal not just reserves, but also conversion efficiency, receptor activity, and mineral regulation. Rather than isolating a single marker, these tests highlight the system at work, showing how vitamin D, calcium, magnesium, and retinol interact as an integrated process. In short, no one number tells the whole story.
🟠 Core Vitamin D Markers
25(OH)D (calcidiol): storage form of vitamin D
1,25(OH)₂D (calcitriol): active, hormone-like form of vitamin D
(Explained in detail above — included here as part of the full panel.)
⚙️ Supporting Minerals
Magnesium RBC: measures magnesium stored inside red blood cells, giving a clearer view of tissue status over several months. In contrast, standard serum magnesium mostly reflects blood levels, which the body keeps tightly regulated even when tissues are depleted. Magnesium is essential for over 300 enzymes, including those that activate vitamin D in the liver and kidneys. Low levels can block vitamin D from working properly, disrupt calcium balance, and contribute to issues like cramps, poor sleep, or anxiety.
Serum calcium: measures total calcium in the blood — including both the protein-bound form and the active free (ionized) form. It doesn’t tell you how much calcium is in your bones or tissues, because blood levels are tightly regulated. If serum calcium is elevated, it may suggest calcium is accumulating in the bloodstream rather than being directed into bone — often a sign of excess vitamin D activity or regulation imbalance.
📡 Regulatory Signals
PTH (parathyroid hormone): regulates calcium and vitamin D balance. When vitamin D is low or calcium intake is insufficient, PTH rises — mobilizing calcium from bone, increasing kidney reabsorption, and activating vitamin D to boost gut absorption. Persistently high PTH may reflect poor vitamin D effectiveness, low calcium, parathyroid disorders, or—less commonly—parathyroid tumors or certain cancers. Low PTH, when calcium is high, may signal excessive vitamin D activity or calcium oversupply.
Retinol (Vitamin A): the active form of vitamin A, found in foods like cod liver oil, liver, and egg yolks. It partners with vitamin D at the receptor so the signal is received. Plant beta-carotene (carrots, sweet potatoes) can convert to retinol, but not always efficiently. Too little weakens vitamin D’s signal; too much can blunt it.
🔍 Case Study: Nancy’s Results
Nancy’s test results tell a bigger story than just “low vitamin D.” Here’s what they show:
- Storage vitamin D (25(OH)D): Low. Her reserves are depleted — the savings account is nearly empty.
- Active vitamin D (1,25(OH)₂D): High. Her body is working overtime to keep blood calcium steady, even though savings are low. This is like living paycheck to paycheck — constant stress on the system.
- PTH (parathyroid hormone): High. Signals that calcium is being pulled from her bones to keep blood levels normal.
- Serum calcium: Normal. It looks fine on paper, but this “normal” is coming at the expense of bone health.
- Retinol (Vitamin A): Low. Without enough vitamin A, vitamin D’s signal doesn’t land well at the receptor, making it harder for her body to use D effectively.
- Magnesium (RBC): Normal. Not the main limiting factor here.
What it means: Nancy doesn’t just have “low vitamin D.” Her body is working hard to compensate — keeping her blood levels steady by pulling calcium from her bones, while weak vitamin A signaling makes the job even harder. It’s like she’s driving with the gas pedal floored just to stay at the speed limit.
Focus for Rebalancing: The first step is safe, steady sunlight to naturally rebuild vitamin D stores. Adding vitamin A–rich foods such as cod liver oil, pastured egg yolks, or liver helps restore receptor balance so vitamin D can do its job more effectively. Maintaining good magnesium intake through diet is also important, with supplementation only if needed.
Other possible patterns
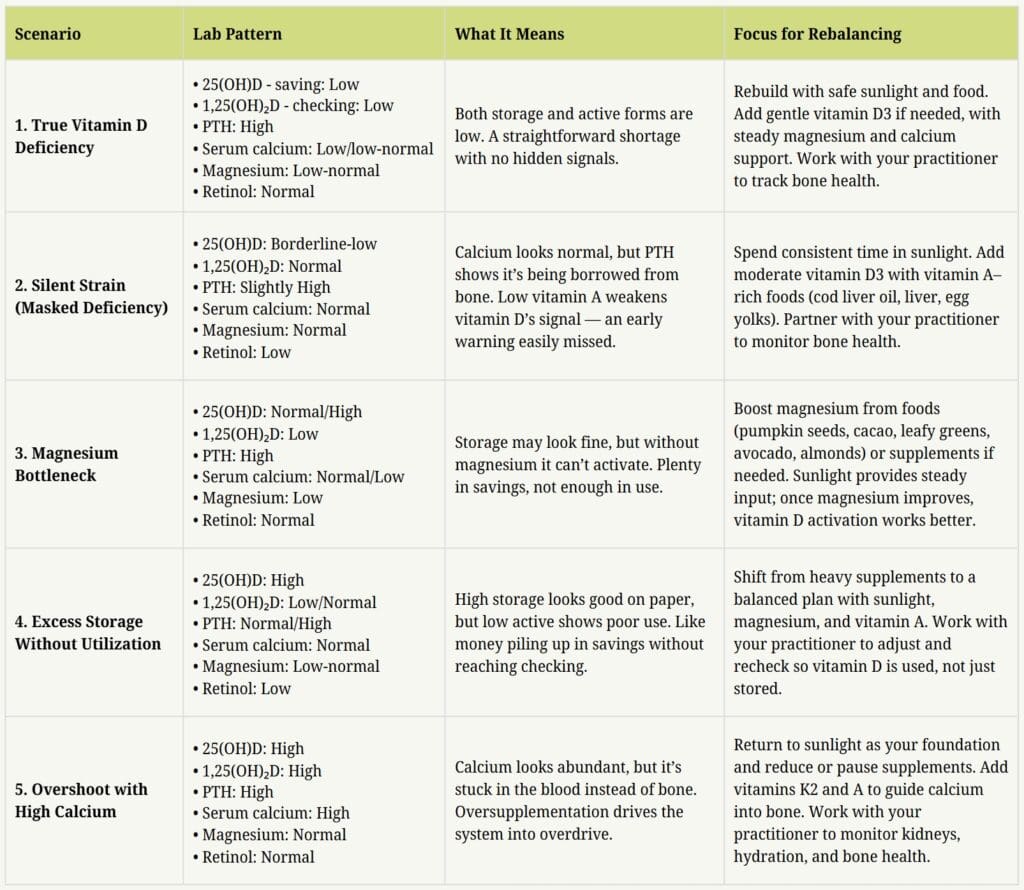
Putting It All Together: These patterns show how the vitamin D–calcium system can shift in different directions depending on storage levels, activation, cofactors, and hormonal feedback. A lab report that looks “low” or “high” may actually reflect a deeper story — from true shortage to blocked utilization or overshoot from over-supplementation. That’s why the most useful insights come from clinical correlation — connecting test results with real-life symptoms and history.
No matter the pattern, the most reliable foundation is safe, regular sunlight exposure. Sunlight provides vitamin D in its natural, self-regulating form, while whole-food sources of cofactors like magnesium, vitamin A, vitamin K2, and B vitamins supply the broader nutrient base. Supplements can then be used strategically, only when needed.
🌞 Sunlight: Nature’s Regulated Delivery System
Sunlight is made of different rays, each with distinct effects and peak timing during the day:
🌅 UVA: present throughout the day; supports blood vessel health and circadian rhythms.
🌞 UVB: peaks around midday; key for vitamin D production in skin.
🔴 Infrared (red/near-infrared/far-infrared): strongest at sunrise and sunset; supports repair and circulation.
Together, these rays form a full spectrum the body has adapted to over millennia. Sunlight works as a package deal — the whole spectrum matters, not just one slice.
When skin is exposed to UVB light, it produces vitamin D, helps sync circadian rhythm, supports vessels, and boosts mitochondrial energy. The process is self‑limiting: once enough vitamin D is made, the excess is photodegraded. [1,2]
By contrast, all documented vitamin D toxicity cases are supplement‑related — not sun‑related. [3]
Smart sunlight habits:
- Start with morning light to build tolerance and support circadian rhythm.
- For vitamin D, aim for midday exposure (when UVB is strongest) on larger skin areas — short enough to avoid burning.
- Increase gradually, especially after winter or illness.
- Protect eyes and skin sensibly; avoid burns.
- Pair UV with red/infrared (dawn, dusk, or devices) to better mimic the solar spectrum.
💡 Sunlamps: Tools, Not Replacements
Sunlamps are artificial light devices designed to mimic parts of the solar spectrum, usually with UVB to trigger vitamin D production in the skin. They can be helpful when sunlight is scarce. However, unlike true full-spectrum sunlight, most lamps don’t provide the complete balance of wavelengths—especially red and infrared—that protect and regulate the skin’s response.
In fact, most consumer sunlamps emit only narrow UVB bands for vitamin D synthesis. While this can support production, they still lack the balancing red and infrared wavelengths found in full sunlight. Without those protective wavelengths, overuse may increase the risk of “delayed burns.”
Examples of categories you may see:
- Medical‑grade UVB lamps often used under dermatology supervision for psoriasis or eczema treatment.
- Home UVB lamps marketed for vitamin D, sometimes paired with red/infrared light for balance.
- Full‑spectrum lamps that provide visible and near‑infrared light, though not always enough UVB for vitamin D.
If you use a lamp:
- Keep sessions short, build slowly.
- Pair with red/infrared exposure.
- Anchor your day with natural outdoor light for circadian alignment.
- Continue to address dietary inflammation (avoid seed oils; choose whole foods and healthy fats).
⚠️ Tools are supplements to nature, not replacements. Always seek professional guidance and note that these examples are educational, not endorsements.
🧬 Genetics and Epigenetics: Blueprint to Lifestyle
Even when diet, sunlight, and labs are accounted for, differences in certain genes can influence how vitamin D works in our bodies. For example, differences in the vitamin D receptor gene (VDR), CYP2R1 (a liver enzyme), and GC (a vitamin D–binding protein) affect how vitamin D is activated, carried in the blood, and used.
- VDR differences change how well cells respond to vitamin D. Some people see stronger improvements in cholesterol or insulin balance with supplementation, while others show only a small rise in 25(OH)D on blood tests. [10]
- CYP2R1 and GC differences help explain why some people consistently test “low” even with good intake or sunlight. [11]
- Context matters: newer studies link these patterns to vitamin D deficiency in people with metabolic syndrome — a cluster of issues like high blood pressure, cholesterol, and blood sugar [12] — and show that weight and diet can make these effects stronger. [13]
Genetics provide the blueprint, while epigenetics act as the dimmer—sunlight, food, stress, and toxins turn that switch up or down. Even vitamin D itself can influence this feedback loop, showing how genes and lifestyle work together.
Practical takeaway: Vitamin D plans are not one-size-fits-all. Our genes are not our destiny — they are a starting point shaped by how we live. If your labs or symptoms don’t match expectations, genetics may be part of the reason, and epigenetics offers a powerful entry point for change.e underscores the importance of personalized, context-driven decisions rather than blanket protocols.
🌐 Closing Thoughts: How to Move Forward Safely
We’ve covered a lot — from sunlight and circadian rhythm to labs, cofactors, and even genetics. All of these pieces show us that vitamin D is powerful, not because it’s just a “nutrient pill,” but because it works like a hormone across many systems. That’s why tinkering with it isn’t always straightforward. The goal isn’t to fear vitamin D or avoid supplementation — it’s to use it with context and balance, recognizing that each of us may respond a little differently.
Think of it like driving: sunlight is the built-in cruise control, while supplements are the accelerator. Cruise control keeps you safe, but the gas pedal requires judgment.
🚩 That’s why we watch for red-flag signals
Your body may be telling you to pause and get guidance if you notice:
- Calcium or kidney issues (such as a history of hypercalcemia, kidney stones, or unusual lab values).
- Unexplained symptoms after high-dose vitamin D (for example, thirst, nausea, confusion, or muscle weakness).
- Complex chronic conditions (like autoimmune illness or ongoing inflammation with paradoxical labs).
If any of these appear, it’s a signal to slow down and seek support. Work with someone who can interpret patterns — not just numbers — and help you build a plan that restores balance.
✨ Simple, Sustainable Steps
Here are a few practical steps you can start with:
- Stabilize the base: protein, minerals (especially magnesium), colorful plants, and healthy fats. [6]
- Rebuild light hygiene: morning light, midday UVB, evening soft light. [1,2]
- Test with intention: 25(OH)D + 1,25(OH)₂D, calcium, PTH, magnesium. [7]
- Use supplements sparingly: short-term, practitioner-guided, with re-testing. [3,4,5,9]
Take-home: Sunlight is your foundation, food is your builder, and testing is your guide. With these three in balance — and with genetics and lifestyle shaping how your body responds — vitamin D becomes a steady ally rather than a gamble.
🌸 Ready to Get Clarity on Your Vitamin D?
Lab numbers tell only part of your story. What really matters is how the pieces fit together — your sunlight, your nutrients, your lifestyle, your story. If you’re unsure where to begin, I’d be honored to walk with you and help you create a safe, balanced plan that supports your story.
👉 Explore ways to work together
📚 References
- Holick, Michael F. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. American Journal of Clinical Nutrition, 2004.
- Vieth, Reinhold. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. American Journal of Clinical Nutrition, 1999.
- Galior, Kornelia, Grebe, Skyler, and Singh, Ravinder. Development of vitamin D toxicity from overcorrection of vitamin D deficiency: a review of case reports. Nutrition in Clinical Practice, 2018.
- Wang, Thomas J., Pencina, Michael J., Booth, Sarah L., et al. Vitamin D and the risk of cardiovascular disease. Circulation, 2008.
- Li, Yan Chun, Kong, Jian, Wei, Ming, Chen, Zhen Fu, Liu, Shao Qun, and Cao, Li Ping. 1,25-Dihydroxyvitamin D₃ is a negative endocrine regulator of the renin–angiotensin system. Journal of Clinical Investigation, 2002.
- Rosanoff, Andrea, Weaver, Connie M., and Rude, Ronald K. Suboptimal magnesium status in the United States: are the health consequences underestimated? Nutrition Reviews, 2012.
- Blaney, Garry P., Albert, Paul J., and Proal, Amy D. Vitamin D metabolic pathways in patients with chronic fatigue syndrome. Inflammation Research, 2009.
- Ghaseminejad-Raeini, Ahmad. Immunomodulatory actions of vitamin D in various immune-related disorders: a comprehensive review. Frontiers in Immunology, 2023.
- Grant, William B., Boucher, Bradley J., Al Anouti, Fatme, et al. Vitamin D and Cardiovascular Disease: A Narrative Review. Nutrients, 2025.
- Al-Daghri, Nasser M., et al. Vitamin D receptor gene polymorphisms modify cardiometabolic response to vitamin D supplementation in T2DM patients. Scientific Reports, 2017.
- Ahn, Jiyoung, et al. Genome-wide association study of circulating vitamin D levels. Human Molecular Genetics, 2010.
- Stroia, Carmina Mariana, et al. Relationship between Vitamin D3 Deficiency, Metabolic Syndrome and VDR, GC, and CYP2R1 Gene Polymorphisms. Nutrients, 2024.
- Stroia, Carmina Mariana, et al. The association of VDR, CYP2R1, and GC gene polymorphisms, dietary intake, and BMI in regulating vitamin D status. Diseases, 2025.

keep browsing
I help women reconnect with their bodies and create lasting wellness with personalized nutrition, functional health, and energy practices—so your body can thrive. Feeling wired yet tired, struggling with fatigue, sleep disruptions, digestive issues, or hormonal imbalances? You’re in the right place.
Meet your coach, Ruth!
You Might Also Like...

Trained immunity is more than boosting or suppressing. Beneath immune responses, the body learns patterns, calibrates inflammation, and coordinates signaling across systems. Understanding the full picture invites a calmer, more balanced way to support immune health.

Chloey’s story is one of patience, prayer, and steady progress. Through diet, therapy, and faith-filled parenting, her family discovered that growth may be slow, but it blossoms when nurtured with love, wisdom, and consistency—offering hope for every step of the journey.

Vitamin D is more than sunshine or supplements. Behind the numbers, your body manages savings and spending accounts, cofactors like magnesium and vitamin A, and patterns that labs help reveal. Seeing the full system makes it easier to choose wisely and stay balanced.
How Can I Support You?
Ruth helps women restore balance, rebuild resilience, and feel at home in their bodies — so they can flourish, feel vibrant, and live fully in every season. She integrates lab insights, energy medicine, and personalized wellness strategies to support each client’s unique path to balance and resilience. While she doesn’t diagnose or treat conditions, she helps uncover lifestyle and environmental factors affecting well-being—and equips women with lasting tools to rebuild their health and confidently support those they love.