Because what’s beneath the surface matters more than what’s flagged on the report.
📚 Table of Contents
Introduction: The Illusion of Precision
Hidden Variability: Gage R&R Meets Functional Lab Testing
Beyond the Range: Why Clinical Correlation Matters Most
Practicing Clinical Correlation: T.R.U.S.T.
🧭 Introduction: The Illusion of Precision
Many people arrive with a stack of lab results—some conventional, some functional lab testing—searching for clarity. A number shows up on a report, and decisions follow. But what if that number doesn’t tell the whole story?
In both engineering and healthcare, test results are often treated as definitive. High or low. Normal or abnormal. But in real life, meaning is rarely that binary. What truly matters is what those numbers mean for you, in your unique context.
Think of lab testing like looking through a lens. Ideally, it offers a clean view of your biology—but reality is often messier. Equipment, handling, timing, even environmental conditions can distort the picture. Like smudges on a camera lens, these variables create noise that can blur the signal.
That’s where Gage R&R, a concept from engineering, becomes relevant. Originally used to assess measurement reliability, it raises a question still vital in functional lab testing today:
Is this number a clear reflection of your biology—or just variability in the tools, timing, or environment?
To truly make sense of labs, we need more than data points—we need context: your biology, timing, and the real-life rhythms that give those numbers meaning.
📌 What We’ll Cover
- Why functional lab testing is sensitive—but not always precise
- How Gage R&R helps uncover variability in lab results
- What “out of range” really means—and why it may not signal dysfunction
- Why your story, stress, and symptoms matter more than the numbers
- How clinical correlation brings lab data into alignment with your lived experience
🔍 Hidden Variability: Gage R&R Meets Functional Lab Testing
I love thinking in systems—seeing how parts connect, where breakdowns occur, and how to build lasting resilience. That mindset has served me across engineering, healthcare, and now in helping others find clarity in complexity. Tools and frameworks can guide us, but the truth is layered and dynamic—too nuanced for any single chart, protocol, or model to fully explain.
Even so, systems thinking gives us tools that help clear the lens. One of these is Gage R&R, short for Repeatability and Reproducibility.
🧪 In simple terms:
Gage R&R asks: Can we trust this measurement?
Is what we’re seeing a real biological shift—or just variation introduced by the process, technology, or technician doing the measuring?
In engineering, a “gage” is any tool used to measure—like a scale, ruler, or sensor. Gage R&R prompts us to ask:
Can we trust the tool? Can we trust the process?
Is the result consistent across time, users, and methods?
🧠 Want to go deeper into the engineering side?
👉 More on Gage R&R here.
🔄 Bringing this lens into functional lab testing
We begin to see results not as final answers, but as outputs of dynamic systems.
That shift helps us ask better questions:
- Is this test sensitive and stable enough to measure what it claims?
- Are the results consistent across time, labs, or technicians—or are we reacting to noise?
🎯 Repeatability and Reproducibility
Repeatability refers to how consistently a test produces the same result when the same person, using the same equipment, runs the same test under similar conditions.
- Example: You check your blood sugar twice in a row with the same glucometer—do the readings match?
Reproducibility refers to how consistently a test produces the same result when different people, using different equipment, run the same test on samples from the same person, collected at similar time.
- Example: Two labs analyze saliva collected the same day—do cortisol results agree?
(Biology is always in motion, but we assume close-in-time samples are similar enough to compare.)
💡 Engineering Insight
Repeatability = variation in the tool
Reproducibility = variation between people or labs
In functional lab testing, this invites us to ask:
Is this result showing true change—or just a ripple from how, when, or by whom it was measured?
When variation from the equipment, environment, or technician overshadows the biological signal we’re trying to detect, the test becomes less capable of reflecting true change.
A result might show up as out of range—not because something is wrong, but because background variability crept in during the testing process.
Your biology may still be in rhythm—it’s just that the test didn’t have the consistency or sensitivity to reflect it.
⚖️ Functional Lab Testing is Sensitive by Design
Functional lab ranges are narrower than conventional ones.
They’re designed to catch subtle shifts before dysfunction sets in—but that same sensitivity can also flag normal fluctuations that aren’t true dysfunction.
It’s like zooming in on a photo: the closer you look, the more things blur. A result may appear “out of range” not because something’s wrong, but because we’re looking too closely.
💡 Making Sense of Functional Labs Variability
Lab results often inform key decisions—whether to adjust supplements, shift diet, support detox, or begin hormone therapy.
But before acting on a number, we need to understand how much weight it truly carries.
That’s where the Gage R&R concept becomes invaluable. It invites us to take a step back and ask smarter questions:
- Is this result meaningful—or could it reflect testing variability?
- Is the shift we’re seeing biological—or just a product of different labs, technicians, or timing?
When repeatability is lacking, even small timing or condition changes can make it difficult to track trends with confidence.
When reproducibility is poor, the same test might lead two practitioners to very different conclusions—resulting in mixed guidance, or interventions that miss the mark.
Instead of reacting to every flagged value, we use Gage R&R thinking to pause, zoom out, and assess whether the data in front of us reflects a reliable pattern—or a one-off ripple in the system.
Because in the end, it’s not about clinging to lab values alone—but about using them as tools in context. That’s how we shift from reactive protocols to personalized, grounded care.
🌪️ External Factors That Influence Test Results
Before interpreting results, it helps to recognize what might distort the measurement process itself. External variability—like tools, timing, or handling—can introduce “noise” that clouds the biological signal.
Here are some common sources of variation during testing:
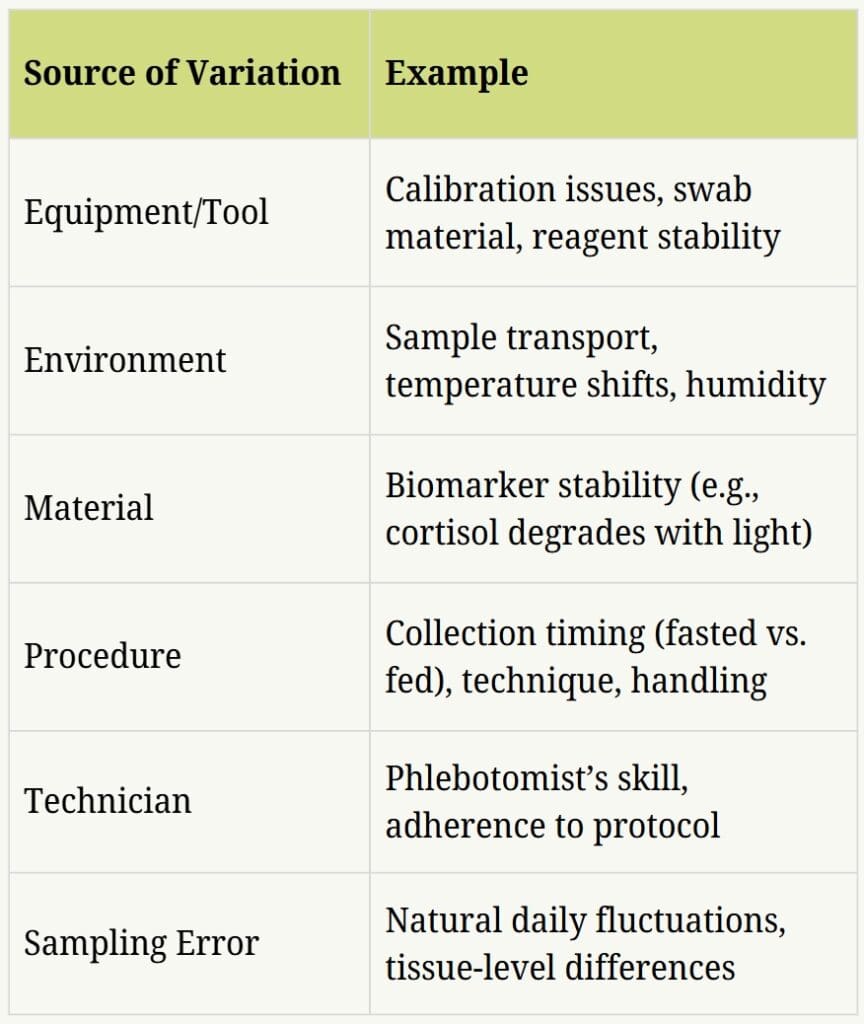
These don’t mean a test is unreliable—but they remind us that measurement precision matters, especially when working within narrow functional ranges.
🌱 Internal Rhythms That Shape Test Results
While external factors shape the quality of the measurement, internal variation is just as important.
What’s happening inside your body—the lived physiology behind the number—can shift what shows up on a test:
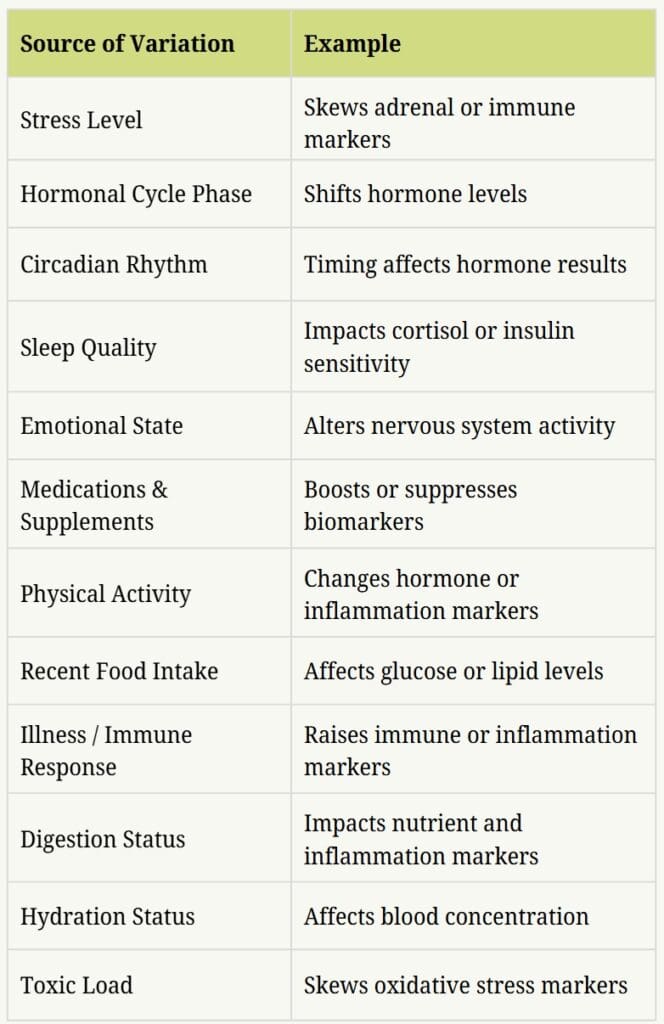
These day-to-day variables can influence cortisol, glucose, digestion, immune markers, and more. They don’t make the test invalid—but they do add context that helps us interpret results wisely.
So instead of asking, “What’s wrong with this number?”—we begin to ask:
- What might have influenced this result?
- Would it look the same next week?
- Does it align with what the person is actually experiencing?
When we see testing as part of a living, responsive system—not just a snapshot—we move from isolated data points to meaningful insight.
So what do we do with all this variability? Rather than reacting to a number in isolation, we turn to clinical correlation—the practice of interpreting lab results within the full picture of the person’s lived experience. This shift helps us move from confusion to clarity, and from reacting to responding. It’s how we start asking better questions… and finding more meaningful answers.
🚦 Beyond the Range: Why Clinical Correlation Matters Most
We’ve seen how test results can be shaped by both external and internal variability—and how even a small shift in timing, stress, or technique can alter the numbers. But what happens when those numbers show up as flagged—marked as High or Low (sometimes just a bolded “H” or “L”) on your lab report?
That’s where things can get confusing—or even unnecessarily alarming.
😌 When a Flagged Result Isn’t a Red Flag
Take a common example: your LDL cholesterol comes back at 132 mg/dL—slightly above the “optimal” threshold. It’s flagged in bold, and suddenly you wonder if something’s wrong.
But what if:
- You weren’t fasted?
- You had coffee with cream that morning?
- You were adjusting to jet lag or recovering from illness?
- You’d just finished a workout?
- You feel well overall—steady energy, clear mind, good sleep?
What matters most is the story behind the number—not the number in isolation. A flagged result doesn’t always mean something’s broken. It may reflect context, timing, or your body’s intelligent response to a shifting environment.
When precision falters, the number loses meaning—unless we bring it back into context.
🌸 Looking Beyond the Number
On paper, Sarah’s cortisol came back high—and she panicked. She feared her adrenals were failing. But when we stepped back and looked beneath the surface, a different story emerged.
She had just flown across time zones, spent several nights with poor sleep, and was navigating a stretch of emotional stress. Her body wasn’t broken—it was adapting. Responding. Protecting her in real time.
The lab result was the tip of the iceberg.
What lay beneath?
- Sleep disruption
- Travel and circadian misalignment
- Emotional stress
- Timing of the test sample
- Nervous system activation
These invisible inputs created a ripple in the result—but not a dysfunction in her biology.
She didn’t need more supplements.
She needed rhythm, rest, and space to recover.
And when that came, her cortisol rebalanced—naturally.

🧊 Lab values show the tip of the iceberg. Sarah’s “high cortisol” wasn’t dysfunction—it was adaptation. What lay beneath? Poor sleep, stress, and circadian disruption. Clinical correlation helps us see what’s really going on.
💡 This is the power of clinical correlation.
It helps us look beyond the numbers, connect the dots, and respond to the whole person—not just what appears above the surface, but the story unfolding beneath it.
🧩 The Power of Clinical Correlation
Sarah’s story reminds us that lab results can reflect adaptation—not dysfunction. Her numbers looked “off,” but her biology was simply responding to life’s demands.
That’s the heart of clinical correlation: connecting what’s on paper with what’s truly happening in real life. It means interpreting lab data through the lens of your real-time symptoms, stressors, and lived experience. This approach helps us:
🚩 Avoid over-treating isolated data points
🤝 Build trust—you are not your lab report
🎯 Tailor care to your biology, not just your biomarkers
Instead of asking, What’s high or low? we ask, What is your body communicating—and how can we support it wisely?
You are not your lab report. Healing happens in the space between the numbers—in your story, your symptoms, and the signals your body is sending.
That’s why, in our work together, lab results aren’t viewed in isolation. They become part of a living conversation with your body—one grounded in curiosity, compassion, and context. We use them to illuminate patterns, not define them—always anchoring interpretation in your lived experience.
We begin by listening to your story. Our intake process explores your symptoms, routines, stressors, environment, and history. From there, we use foundational labs to assess how your systems are functioning—looking at hormones, digestion, detox pathways, energy production, and more.
No single marker gives the full picture. Like the tip of an iceberg, what appears on a lab report is just a glimpse of what’s happening beneath the surface. To understand the whole, we connect the dots across multiple systems—and across your physical, mental, emotional, spiritual, and energetic layers of your physiology.
Zooming out with this integrative lens helps us understand not just what’s happening—but why—so we can support your body’s next best step.
🌺 Practicing Clinical Correlation: T.R.U.S.T.
When your lab results arrive—whether marked as “optimal” or “out of range”—it’s easy to feel reactive. But numbers are only part of the story. Before drawing conclusions or reaching for a fix, you’re invited to practice something deeper: T.R.U.S.T.
This gentle framework helps you shift from reacting to reconnecting—so your next step is guided not just by data, but by the wisdom of your lived experience.
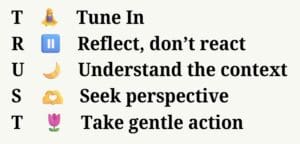
🧘♀️ T — Tune in
Begin with presence. Before analyzing the numbers, take a quiet moment. Breathe. Notice what your body is communicating—not just today, but across the past few days, weeks, or even months. What sensations, emotions, or signals have been showing up? What patterns do you feel in your energy, mood, sleep, or digestion?
Tuning in grounds you in your inner reality—not just external data.
If you sense your energy is out of sync but labs haven’t caught up, the Daily Energy Routine (DER) can help you reconnect to your energetic baseline.
🫖 R — Reflect, don’t react
It’s natural to feel something when a value is flagged or outside the ideal range. But instead of labeling it as “bad” or rushing to fix it, pause. Ask yourself: What might this be reflecting?
Lab results are snapshots in time. By reflecting first, you make room for nuance, compassion, and clinical correlation.
🌙 U — Understand the context
Zoom out. Had you been traveling? Grieving? Caregiving? Navigating stress or sleep disruption? These events can influence lab results—sometimes weeks before a test.
Often, imbalances begin on the energetic or emotional level before they manifest physically. If that resonates, you may find clarity in my 2-part blog series, beginning with The Seasons Within: Hormonal Health Across Her Life, which explores how life transitions, stress, and rhythm disruption shape hormonal health—often long before they show up in lab data.
If you menstruate, consider your cycle phase at the time of testing—pre-period fatigue, hormone shifts, or ovulatory surges may alter markers like cortisol or inflammation.
Also revisit any tracking data: food logs, sleep journals, symptom diaries. Do the results align with what you’ve been noticing?
🫶 S — Seek perspective
You don’t have to navigate your results alone. Reach out to someone who knows your journey—a coach, practitioner, or trusted friend. Speaking your observations aloud often reveals hidden insights. And others may reflect patterns you’ve missed.
If your results feel unclear or overwhelming, you don’t have to figure them out alone. My Specialty Lab Review offers a space to explore your numbers gently and in context—so your next step feels grounded, not rushed.
🌷 T — Take gentle action
Instead of rushing into protocols, ask: What is my body ready for? Maybe it’s more sleep, deeper hydration, a pause from caffeine, or emotional boundaries. Start small. What you shift with grace is often more sustainable than what you fix with force.
And if something feels too tangled or heavy to navigate alone—that’s your body’s way of asking for support. Real healing happens in relationship, not isolation. If you’re longing for guidance that honors your biology, your story, and your pace, I invite you to explore the 90-Day Wellness Journey—a space designed to help you integrate lab results, restore rhythm, and reconnect with the wisdom of your body.
Practicing clinical correlation is less about fixing what’s on the page and more about reconnecting with what’s unfolding in real life. When you begin with T.R.U.S.T., you start to walk alongside your body—not just follow the numbers—and that’s where meaningful change begins.
🗺️ Conclusion: The Map Is Not the Terrain
What your labs reveal matters—but how you meet that information matters more.
We’ve seen that functional lab testing isn’t always as precise or clear-cut as it appears. Hidden variability, personal rhythms, and life context all shape what shows up on paper. Practicing clinical correlation means interpreting results through presence, not panic—and letting your story inform the meaning behind the numbers.
Lab results can guide us, but they’re not the whole journey. They’re the map, not the terrain.
A map offers points and paths, but it can’t capture the feel of the forest floor or the wind in the trees. Your terrain is your body: living, dynamic, and constantly responding to real-time experience.
A lab report is only a sliver of the full landscape—a tip-of-the-iceberg glimpse. It reflects a moment, not the full movement.

When the terrain differs from the map, trust the terrain. Lab results can point the way—but they don’t always reflect the full reality of your body in motion. Symptoms, stress, cycles, and real-life rhythms shape the path forward.
As Gage R&R reminds us, measurement isn’t always truth—it’s a reflection shaped by tools, timing, and context. The more we honor those layers, the clearer our path forward becomes.
That’s why we don’t treat labs in isolation. We listen to your story—your symptoms, history, patterns, stressors, cycles, and lived experience. We connect the dots and consider the full context.
What seems “out of range” may be a wise adaptation. What looks “normal” might be masking deeper depletion. Lab values are never the full story—they’re just one part of it.
We shift the question from diagnosis to dialogue.
✨ What is your body trying to say?
✨ And how can we meet it with insight, curiosity, and care?
Because real healing doesn’t happen on paper. It happens in real time—in relationship with your body, your choices, and your story.
🪷 Ready to Look Beyond the Numbers?
If you’ve ever been told your labs are “normal” but still felt something was off—you’re not alone. You’re exactly who this article was written for.
Too often, we’re handed data without insight. But numbers are just one part of the story.
If you’re ready to understand your lab results in the context of your symptoms, rhythms, and lived experience—I’d be honored to support you.
Whether you’re curious about a Specialty Labs Review or exploring a deeper Wellness Journey, you’re warmly invited to connect.

keep browsing
I help women reconnect with their bodies and create lasting wellness with personalized nutrition, functional health, and energy practices—so your body can thrive. Feeling wired yet tired, struggling with fatigue, sleep disruptions, digestive issues, or hormonal imbalances? You’re in the right place.
Meet your coach, Ruth!
You Might Also Like...

Trained immunity is more than boosting or suppressing. Beneath immune responses, the body learns patterns, calibrates inflammation, and coordinates signaling across systems. Understanding the full picture invites a calmer, more balanced way to support immune health.

Chloey’s story is one of patience, prayer, and steady progress. Through diet, therapy, and faith-filled parenting, her family discovered that growth may be slow, but it blossoms when nurtured with love, wisdom, and consistency—offering hope for every step of the journey.

Vitamin D is more than sunshine or supplements. Behind the numbers, your body manages savings and spending accounts, cofactors like magnesium and vitamin A, and patterns that labs help reveal. Seeing the full system makes it easier to choose wisely and stay balanced.
How Can I Support You?
Ruth helps women restore balance, rebuild resilience, and feel at home in their bodies — so they can flourish, feel vibrant, and live fully in every season. She integrates lab insights, energy medicine, and personalized wellness strategies to support each client’s unique path to balance and resilience. While she doesn’t diagnose or treat conditions, she helps uncover lifestyle and environmental factors affecting well-being—and equips women with lasting tools to rebuild their health and confidently support those they love.